Saving Smiles: Exploring Root Canals and the Promise of Vital Pulp Therapy
- naytoghlo
- Apr 18, 2025
- 5 min read
Updated: Apr 19, 2025

As practitioners, we're constantly evaluating the most effective and conservative approaches for managing pulpal pathosis. Recent discourse in the endodontic community highlights the spectrum of treatment options, ranging from the predictable, time-tested root canal procedure to the evolving concepts of vital pulp therapy. Let's delve into insights gleaned from recent clinical case discussions to enhance our understanding and treatment planning strategies.
Root Canal Therapy: Mastering the Fundamentals
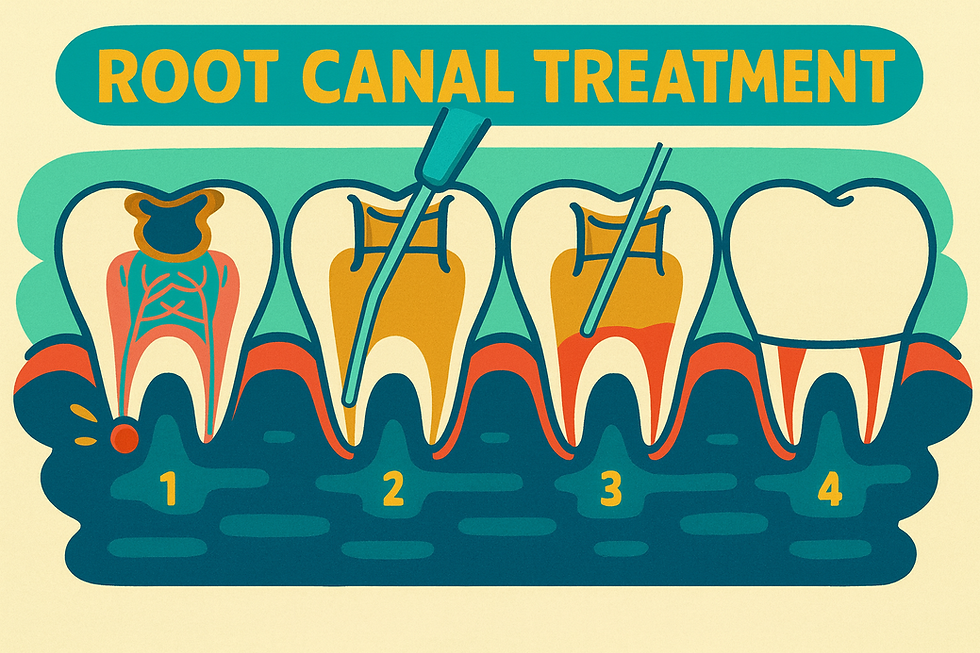
A cornerstone of our practice, the root canal procedure aims to address teeth with infected or necrotic pulps through meticulous cleaning, shaping, and obturation of the root canal system. A comprehensive case by Dr. Samuel R. Johnson presentation on an upper left seven (UL7) demonstrates the critical steps involved:
Accurate Diagnosis and Access: Initial assessment, often involving radiography, is crucial to determine the pulpal status. In the presented case, a significant radiolucency suggested necrosis or irreversible pulpitis. Establishing proper access through the coronal aspect of the tooth is the first surgical step.
Canal Negotiation and Working Length Determination: Identifying and navigating all canals (palatal, mesiobuccal, distobuccal, and potentially MB2 in maxillary molars) with fine instruments like a size 10K file is essential. Determining the accurate working length, often with the aid of an electronic apex locator, ensures instrumentation remains within the canal space. The operator in the video emphasizes the tactile sensation of gently passing the file through the apex and retracting slightly to establish this length.
Glide Path Creation and Canal Shaping: Utilizing glide path files (e.g., 15/.03 High Flex) prepares a smooth pathway for subsequent shaping instruments. Master apical files (e.g., 25/variable taper High Flex) are then used to create a defined shape to the working length or slightly short of it (e.g., 0.5mm). The importance of copious irrigation with sodium hypochlorite throughout instrumentation is highlighted for disinfection and debris removal. Recapitulation with a small K-file ensures canal patency.
Disinfection Protocols: Beyond irrigation, the disinfection phase may involve the use of EDTA to remove the smear layer and potentially the disinfection of hand files. Final irrigation protocols with sodium hypochlorite, sometimes activated ultrasonically, are crucial for eliminating residual bacteria. The operator emphasizes irrigating until the irrigant remains clear.
Obturation: Following thorough drying of the canals with paper points, obturation with gutta-percha and sealer aims to create a fluid-tight seal. Techniques include fitting the gutta-percha cone to the working length with tactile "tug back", using heated pluggers to remove excess gutta-percha, and vertical condensation with pluggers like a Machtou. Post-operative radiographs confirm the adequacy of the fill.
The presented case also underscores practical considerations like the strategic use of a 30-minute initial appointment for assessing restorability, providing initial pain relief, and easing patient anxiety, potentially simplifying the subsequent root canal appointment. The unwavering emphasis on rubber dam isolation as a non-negotiable standard for disinfection and medicolegal protection is also paramount.
The Evolving Landscape: Vital Pulp Therapy and Adult Pulpotomy
While root canal therapy boasts a high success rate, the concept of preserving vital pulp tissue in cases of early irreversible pulpitis is gaining renewed attention. Vital pulp therapy, including procedures like direct pulp capping and pulpotomy, aims to capitalize on the pulp's inherent healing potential.
Dr. Nasseh's discussion on adult pulpotomy provides valuable insights into this less conventional approach, while explicitly stating that it is not currently considered standard of care as a definitive treatment in the US. The presented case of a lower second molar with symptomatic irreversible pulpitis (lingering pain, spontaneous pain, but negative to percussion) illustrates a specific protocol:
Careful Diagnosis: Selection criteria are crucial, with early irreversible pulpitis and a normal apical diagnosis being key factors in considering this approach.
Meticulous Decay Removal and Isolation: Complete removal of decay, minimizing the risk of bacterial contamination, followed by strict rubber dam isolation (potentially using a double rubber dam technique to minimize aerosol contamination) are essential.
Coronal Pulpotomy: Removal of the entire coronal pulp with a sterile bur, followed by achieving hemostasis, is the core of the procedure. Various hemostatic agents can be employed, including dilute sodium hypochlorite or hypertonic saline. Dr. Nasseh also explored a novel cryotherapy technique using endo ice applied to a hypertonic saline-soaked pellet to aid in hemostasis and reduce inflammation, emphasizing this as an original, yet unpublished, technique.
Biocompatible Medicament Placement: A bioceramic putty (e.g., EndoSequence BC Putty) is placed directly over the radicular pulp stumps to promote healing and create a seal. This is then covered with a liner (e.g., EndoSequence BC Liner) for bulk filling and provisional restoration. The strong bonding observed between the putty and liner after eight weeks in the presented case is noteworthy.
Delayed Root Canal Completion (in the US context): Due to the current standard of care in the US, these cases are typically followed by a complete root canal procedure after a period of monitoring (e.g., eight weeks). This delay allows for assessment of the pulpotomy's short-term success based on patient symptoms. The presented case showed vital pulp tissue remaining after eight weeks beneath the bioceramic putty, highlighting the potential for pulp preservation.
Here are the clinical steps of Dr. Nasseh's investigational adult pulpotomy protocol:
Primary isolation with a rubber dam and complete removal of decay.
Secondary isolation by placing a second rubber dam.
Full coronal pulpotomy using a new, sharp bur.
Achieving hemostasis with sodium hypochlorite or hypertonic saline, or Dr. Nasseh's novel cryotherapy technique using refrigerant on a saline-soaked cotton pellet.
Placement of a 1-2 millimeter layer of bioceramic putty over the pulp stumps.
Bulk-filling the remaining coronal space with a bioceramic liner and light-curing.
Eight-week follow-up to monitor symptoms.
Completion of root canal therapy during the second appointment.
Key Considerations for the Practitioner
Several critical points emerge for us as clinicians considering these treatment modalities:
Diagnostic Accuracy Remains Paramount: As Dr. Nasseh emphasizes, accurately diagnosing the pulpal and apical status is a significant limitation in vital pulp therapy. Our current diagnostic tools provide indirect assessments, and the true histological condition of the pulp remains unknown until access is gained.
Standardized Protocols are Evolving: While adult pulpotomy shows promise in select cases, universally accepted clinical protocols are still under investigation. The protocol described by Dr. Nasseh represents one such attempt to optimize outcomes.
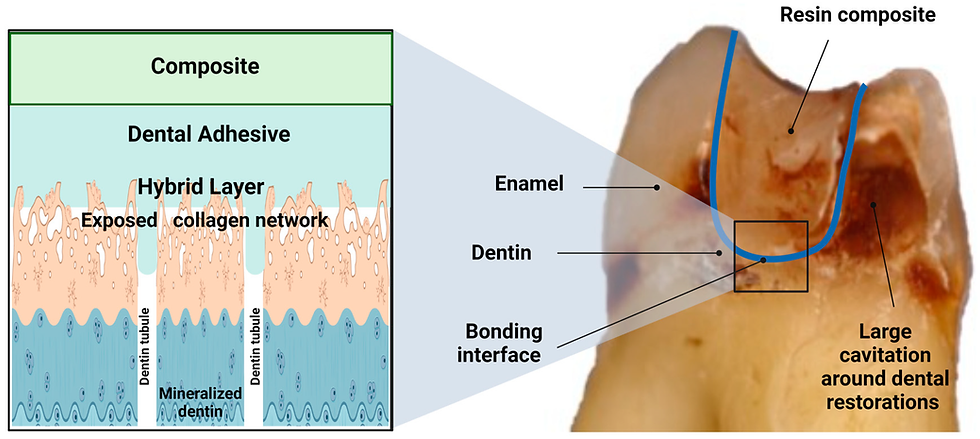
Material Science Plays a Crucial Role: Advancements in biocompatible and bioactive materials, such as bioceramic sealers and putties, are integral to the potential success of vital pulp therapy by promoting healing and reducing inflammation.
Adult Pulpotomy: A Provisional Measure in the US: It is crucial to reiterate that, currently, adult pulpotomy is not considered a definitive treatment under the standard of care in the US. Therefore, proceeding with complete root canal therapy following a period of monitoring is generally necessary to meet legal and ethical obligations.
Conventional RCT Remains the Gold Standard: Despite the interest in vital pulp therapy, conventional root canal therapy will undoubtedly remain the primary treatment for teeth with more advanced pulpal disease or necrosis. Adult pulpotomy is presented as a niche procedure, not a replacement for RCT.
Patient Education and Prevention are Key: Ultimately, our efforts should also focus on educating patients about the importance of oral hygiene, diet, and timely intervention to prevent pulpal disease in the first place, potentially reducing the need for more invasive procedures.
Conclusion
The field of endodontics continues to evolve, with a growing emphasis on biologically driven treatment approaches. While meticulous root canal therapy remains a cornerstone of our practice, vital pulp therapy, particularly adult pulpotomy, offers a glimpse into potentially more conservative interventions for carefully selected cases. As we navigate these options, a thorough understanding of the underlying principles, procedural nuances, and current limitations is essential to providing the best possible care for our patients. Further research and the development of standardized, predictable protocols will be crucial in defining the future role of vital pulp therapy in our clinical armamentarium.
Dr. Noor N. AyToghlo

Comments